Managing Achilles Tendon Injuries
Achilles Tendon Anatomy
Types of Injury: Insertional Tendinitis
Types of Injury: Paratenonitis
Types of Injury: Non-insertional Tendonosis
Avoiding Achilles Injuries
Despite its broad width and significant length, runners injure their Achilles tendons with surprising regularity. In a recent study of 69 military cadets participating in a six-week basic training program that included distance running, 10 of the 69 trainees suffered an Achilles tendon overuse injury(1).
The prevalence of this injury is easy to understand when you consider the tremendous strain runners place on this tendon; for example, during the push-off phase of the running cycle, the Achilles tendon is exposed to a force of seven times bodyweight(2). This is close to the maximum strain the tendon can tolerate without rupturing(3). Also, when you couple the high strain forces with the fact that the Achilles tendon significantly weakens as we get older, it is easy to see why this tendon is injured so frequently.
To help you more clearly understand the mechanisms associated with the various types of Achilles tendon injuries, this article will briefly review the tendon’s functional anatomy, and then relate this information to the different types of Achilles injuries and their respective treatments.
Achilles Anatomy
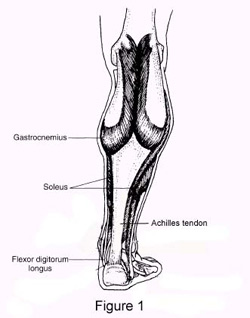
Anatomically, the Achilles tendon represents the conjoined tendons of the gastrocnemius and soleus muscles. A small, thin muscle called plantaris runs between the gastroc and soleus, but it is technically not considered part of the Achilles tendon. The gastrocnemius is the two-headed surface muscle that bulges when you stand on your toes, while the soleus lies deep to the gastroc. The main difference between these two muscles is that the gastroc originates from above the knee joint, while the soleus attaches along the back of the leg and does not cross the knee. As a result, they are stretched and exercised differently.
Approximately five inches above the Achilles attachment to the back of the heel, the tendons from gastroc and soleus unite to form a single thick Achilles tendon (see Figure 1). These conjoined tendons are wrapped by a single layer of cells called the paratenon. This sheath-like envelope is rich in blood vessels necessary to nourish the tendon. The tendon itself is made primarily from two types of connective tissue, known as type-1 collagen and type-3 collagen. In a healthy Achilles tendon, 95 percent of the collagen (which accounts for 70 percent of the dry weight of the tendon) is made from type-1 collagen, which is stronger and more flexible than type 3. It is the strong crosslinks and parallel arrangement of the type-1 collagen fibers that gives the Achilles tendon its strength.
The Achilles tendon is unique in that, at about the point where the gastroc and soleus muscles unite, the tendon suddenly begins to twist, rotating a full 90 degrees before it attaches to the back of the heel. This extreme twisting significantly improves efficiency in running, as it allows the tendon to function as a spring, absorbing the gravitational energy present during the early phases of the gait cycle and returning the energy in the form of elastic recoil during the propulsive period. In fact, recent research has demonstrated that the gastroc and soleus muscles perform relatively little work during the propulsive period. Rather than acting as small motors that propel the body forward (as had been previously suggested), it appears that the primary role of these muscles is to hold the ends of the Achilles tendon rigid so that the tendon itself can store and return energy like a strong rubber band.
The belief that muscles act merely to adjust tension on spring-like tendons was first demonstrated in a study by Roberts and colleagues published ten years ago(4). These researchers surgically implanted special crystals and strain gauges into the gastroc muscles and Achilles tendons of turkeys that were forced to run on treadmills.
They noted that as the turkeys ran at faster speeds, there was little change in muscle length (approximately 7 percent change with each stride), and the muscles generated just enough force to keeps the tendons stretched, thereby allowing the tendons to store gravitational energy. By calculating muscle activity and force production, the researchers demonstrated that storing and recovering energy in the stretched tendons were responsible for more than 60 percent of the work performed by the muscle-tendon complex.
The results of this study make it clear that the spring-like action of the Achilles tendon acts to significantly lessen the metabolic expense of running by reducing the work load on the muscles (which consume calories, generate heat and require removal of waste products such as lactic acid). By passively storing and returning energy, the Achilles tendon allows the leg to behave like a very efficient pogo stick.
Injuries to the Achilles Tendon
In spite of its clever design and significant strength, the extreme forces it is exposed to cause the Achilles tendon to break down all too frequently. Depending on the location of the damage, Achilles tendon overuse injuries are divided into several categories: insertional tendinitis, paratenonitis and non-insertional tendinosis.
Insertional Tendinitis
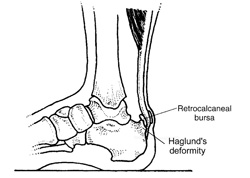
As the name implies, insertional tendinitis refers to inflammation at the attachment point of the Achilles on the heel. This type of Achilles injury typically occurs in high-arched, inflexible individuals, particularly if they possess what is known as a Haglund’s deformity, a bony prominence near the Achilles attachment on the heel. Because a bursa is present near the Achilles attachment (bursae are small sacs that contain lubricants that minimize the shearing of the tendon against the bone), it is very common to have an insertional tendinitis with the retrocalcaneal bursitis (see Figure 2).
Until recently, the perceived mechanism for the development of insertional tendinitis was pretty straightforward: an individual with a tight gastroc/soleus who runs regularly creates an increased tensile strain that causes the Achilles tendon to break down where the pulling force is the greatest.
While this makes perfect sense, recent research has shown that just the opposite is true(5). By placing strain gauges inside different sections of six cadeveric Achilles tendons and loading the tendons with the ankle positioned in a variety of angles, researchers from the University of North Carolina discovered that the back portion of the Achilles tendon is exposed to far greater amounts of strain (particularly as the ankle was moved upward), while the forward section of the tendon, which is the section most frequently damaged with insertional tendinitis, was exposed to very low loads. The authors suggest that the lack of stress on the forward aspect of the Achilles tendon (which they referred to as a tension-shielding effect) may cause that section to weaken and eventually fail.
Accordingly, treating an Achilles insertional tendinitis should involve strengthening the forward-most aspect of the tendon. This can be accomplished by performing a series of eccentric load exercises (these will be discussed briefly) with the ankle placed through a full range of motion. It is particularly important to work the Achilles tendon with the ankle maximally plantarflexed (i.e., standing way up on tip toes), as this position places greater amounts of strain on the more frequently damaged anterior aspect of the tendon.
In addition to the eccentric exercises, another effective treatment is lateral heel wedges. These wedges, which are pasted to the outer portion of an insole, are typically used with high-arched individuals, and function to pronate the foot inward, thereby redistributing tensile strains throughout the attachment of the Achilles tendon. Heel lifts are always a consideration, but be careful-they may feel good at first, but the calf muscles quickly adapt to their shortened positions, thereby minimizing the positive effect of the heel lift. Heel lifts also increase stress on the sesamoid bones (small bones under the inner forefoot) and the plantar fascia, and should therefore be used with caution, as it’s not uncommon to trade one injury for another.

The final consideration in treating insertional Achilles tendinitis relates to the forward pitch of the running shoe’s heel counter. (This is the back upper portion of the shoe that touches the Achilles tendon.) Over the past few years, for no clear reason, many running shoe manufacturers have added a forward angulation to the upper portion of the heel counter that causes it to project directly into the Achilles tendon. This addition often pushes directly into the back of the Achilles insertion, causing chronic inflammation, particularly if a Haglund’s deformity is present.
Treatment in this situation is to look for running shoes that do not contact the Achilles insertion. Unfortunately, such shoes are few and far between. A simple alternative is to cut off the upper back section of the heel counter so that it no longer touches the tendon. This is not as difficult as it sounds, and can usually be done with a standard bread knife. (Face the shoe and knife away from you as you make this cut.) I usually remove the upper third of the heel counter.
Paratenonitis
The next type of Achilles tendon overuse injury is paratenonitis. This injury, which is very common in runners, represents an inflammatory reaction in the outer sheath of cells that surround the tendon. Over-pronators are particularly prone to this injury, as rapid pronation creates a whip-like action that can damage the tendon sheath, particularly the inner side.
The first sign of the injury is a palpable lump that forms about two inches above the Achilles attachment. This mass represents localized thickening in response to microtrauma. If you continue running, the size of the lump increases and eventually becomes so painful that running is no longer possible.
Treatment for Achilles paratenonitis is to immediately reduce the swelling with frequent ice packs. If you pronate excessively, make sure you’re wearing an appropriate motion-control shoe. You might also want to consider trying orthotics. (Start with over-the-counter models.) Night braces are also effective with paratenonitis, as tissues immobilized in a lengthened position heal more quickly.
If caught in time and the problem is corrected, Achilles paratenonitis is no big deal. However, if untreated, this injury may turn into a classic Achilles non-insertional tendinosis. This injury involves degeneration of the tendon approximately one to two inches above the attachment on the heel. Because this section of the tendon has such a poor blood supply, it is prone to injury and tends to heal very slowly.
Non-insertional Tendinosis
Unlike insertional tendinitis and paratenonitis, non-insertional tendinosis represents a degenerative noninflammatory condition. (The suffix “osis” refers to morbid degeneration, while “itis” refers to inflammation.) Apparently, repeated trauma from running causes cells such as fibroblasts to infiltrate the tendon, where, in an attempt to heal the injured regions, they begin to synthesize collagen. In the early stages of tendon healing, the fibroblasts manufacture almost exclusively type-three collagen, which does the job, but is relatively weak and inflexible compared to the type-one collagen found in healthy tendons. If everything goes right, as healing progresses, greater numbers of fibroblasts appear and collagen production shifts from type three to type one.
Unfortunately, many runners don’t give the tendon adequate time to remodel, which can take up to six months. In this case, a series of small partial ruptures begin to occur that can, paradoxically, act to lengthen the tendon, thereby resulting in increased range of upward motion at the ankle. At this point, pain is significant, and the runner is usually forced to stop running altogether.
Various factors may predispose you to developing non-insertional tendinosis. In the study of military recruits mentioned at the start of this article, the recruits developing Achilles injuries were too flexible (they had greater than 10 degrees of ankle dorsiflexion) and had calf weakness. It is likely that these two factors cause a whipping action that can damage the weakened tendons.
The good news about non-insertional tendinitis is that there is a new treatment protocol that has excellent success, even with some of the worst injuries. Referred to as heavy-load eccentric exercises, this treatment protocol involves placing a weighted backpack on your back while standing on the edge of a stair with your heels hanging off the stair. Using both legs, you raise your heels as high as possible, and then remove the uninjured leg from the stair. The injured leg is then gradually lowered through a full range of motion. The uninjured leg is then placed back on the stairway, and both legs are again used to raise the heels as high as possible. Three sets of 15 repetitions are performed twice a day with the knees both straight and bent. In a 12-week study of 15 recreational runners with chronic Achilles non-insertional tendinosis, Swedish researchers had a 100-percent success rate at treating this difficult injury(6). The 100-percent success rate was impressive given that these were older athletes (average age 45) who had had symptoms for almost two years and had failed with every prior treatment protocol, such as nonsteroidal anti-inflammatory drugs, orthotics and physical therapy.
Besides the heavy-load eccentric exercises, another effective and readily available method for improving Achilles function is deep tissue massage. The theory is that aggressive massage breaks down the weaker type-three collagen fibers and increases circulation so that healing can occur.
To test this theory, researchers from the Biomechanics Lab at Ball State University(7) surgically damaged the Achilles tendons of different groups of rats. In one group, an aggressive deep tissue massage was performed for three minutes on the 21st, 25th, 29th and 33rd day post injury. Another group served as a control. One week later, both groups of rats had their tendons evaluated with light and electron microscopy. Not surprisingly, the tendons receiving deep tissue massage showed increased fibroblast proliferation, which would create an environment favoring repair of the tendon.
A more high-tech method of breaking down scar tissue involves extracorporeal shock wave therapy. This technique involves using expensive machinery that blasts the Achilles with high-frequency sonic vibrations. Recent research has shown comparable outcomes between shock wave therapy and heavy-load eccentric exercises in treating non insertional Achilles tendinosis(8). As result, this expensive method of treatment should be used only after conventional methods have failed.
Avoiding Achilles Injuries
Regardless of whether the Achilles injury is insertional or non-insertional, a great method for lessening stress on the Achilles tendon is flexor digitorum longus exercises. This muscle, which originates along the back of the leg and attaches to the tips of the toes, lies deep to the Achilles. It works synergistically with the soleus muscle to decelerate the forward motion of the leg before the heel leaves the ground during propulsion. This significantly lessens strain on the Achilles tendon as it decelerates elongation of the tendon.
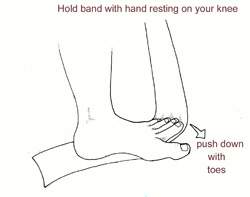
Many foot surgeons are aware of the connection between flexor digitorum longus and the Achilles tendon-surgical lengthening of the Achilles (which is done to treat certain congenital problems) almost always results in developing hammer toes as flexor digitorum longus attempts to do the job of the recently lengthened tendon. The exercises are simple to perform and require using a small piece of Thera-Band (see Figure 3). I recommend three sets of 40 repetitions performed daily.
I also recommended that the runner forcefully curl the toes downward into the insole during the push-off phase of the running cycle. This naturally strengthens the flexor digitorum longus muscle, thereby lessening strain on the Achilles tendon. It is easy to see if you have weakness in this muscle by looking at the insole of your running shoes. Normally, when the flexor digitorum muscle is strong, you will see well-defined indents beneath the tips of the second through fifth toes. In contrast, a weak flexor digitorum produces no marks beneath the toes and shows signs of excessive wear in the center of the forefoot only.
Finally, avoid having cortisone injected into either the bursa or tendon-doing so weakens the tendon as it shifts production of collagen from type one to type three. In a recent study published in the Journal of Bone Joint Surgery(9), cortisone was shown to lower the stress necessary to rupture the Achilles tendon, and was particularly dangerous when done on both sides, as it produced a systemic effect that further weakened the tendon.
To sum up, here is an overview of managing Achilles tendon disorders: warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you are overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
All illustrations in this article reproduced, with permission, from: Michaud TC. Foot Orthoses and Other Forms of Conservative Foot Care.
References:
(1) Mahieu NN, Witvruow E, Stevens V, et al. Intrinsic risk factors for the development of Achilles tendon overuse injuries. Am J Sp Med 2006;34(2):226-35.
(2) Schepsis A, Jones H, Haas A. Achilles tendon disorders in athletes. Am J Sp Med 2002;35(2):287-305.
(3) Allenmark C. Partial Achilles tendon tears. Clin Sports Med 1992;11:759-769.
(4) Roberts TJ, Marsh RL, Weyand PG, Taylor CR. Muscular force in running turkeys: the economy of minimizing work. Science 1997;Feb(275):1113-15.
(5) Lyman J, Weinhold P, Almekinders LC. Strain behavior of the distal Achilles tendon. Am J Sp Med 2004;32(2):457-61.
(6) Alfredson H, Pietila T,Jonsson P et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sp Med 1998;26(3):360-6.
(7) Davidson CJ, Ganion LR, Gehlsen GM, et al. Rat tendon morphological and functional changes resulting from soft tissue mobilization. Med Sci Sp Exerc 1997;29(3):313-19.
(8) Rompe J, Nafe B, Furia J. Eccentric loading, shock wave treatment or a wait-and-see policy for tendinopathy of the main body of tendo Achilles. Am J Sp Med 2007;35(3):374-83.
(9) Hugate R, Pennypacker J, Saunders M, Juliano P. The effects of intratendinous injections of corticosteroid on the biomechanical properties of rabbit Achilles tendons. JBJS (American)2004;86:794-801.
Updated May 3, 2018
Updated May 28, 2015
Updated November 8, 2014
Posted April 2007
- Posted May 28, 2015
© Copyright 2007-2024 by Take The Magic Step®. All Rights Reserved.